Managing the complications caused by surgical procedures in patients with incontinence were examined in the second and last day of the 3rd EAU Baltic Meeting with experts warning not only about the severity but also the complexity of complications.
Topics discussed by speakers Martin Kivi (EE), Ulo Zirel (EE), Zane Pilsetniece (LV) and Marija Barisiene (LT) were male slings surgery, sphincter prosthesis, complications management after female sling surgery and pelvic floor reconstruction, respectively.
Kivi gave an overview of the pathophysiology of male incontinence and looked into the current treatment options in stress urinary incontinence (SUI) such as compression devices, fixed male slings (FMS) and gave pointers in support optimisation.
“SUI and erectile dysfunction (ED) are the most common adverse consequences of radical prostatectomy. At 12-month post-prostatectomy, 5 to 10% of men may still experience SUI,” said Kivi.
Artificial urinary sphincter (AUS) is accepted as standard for the surgical treatment of persistent SUI, according to Kivi, and noted that around a third of patients after AUS require surgical repair within 10 years. He mentioned treatment options such as AdVance which reported overall success rates ranging from 54.5% to 90.6% and cure rate of around 51.4% to 73.7%.
Zirel examined the various indications for AUS such as post-prostatectomy incontinence, sphincteric dysfunction and neurogenic bladder. “All patients must have sufficient sophistication and hand functionality to operate the pump,” noted Zirel, while underscoring the incidence of infections, cuff erosion, tissue atrophy and mechanical failure.
Pilsetniece spoke on how to manage complications resulting from female sling surgery such as urinary retention, intra-operative bladder perforation, urethral injury, bleeding and sling extrusion/erosion, among others.
“Injury of the urethra or bladder during vaginal dissection is best avoided by placing a urethral catheter or emptying the bladder,” she said. She added that avoiding excessive sling tension and using intraoperative cystourethroscopy also help reduce the incidence of injuries.
Pilsetniece: “Intraoperative cystourethroscopy is always indicated to rule out urethral or bladder perforation, whether the sling is placed through a retropubic or a transobturator approach.”
In her take-home message she stressed that a comprehensive evaluation of the problem is crucial. “Before making a decision, evaluate the problem comprehensively, discuss the risks and benefits with a patient, as well as any possible alternative treatments.”
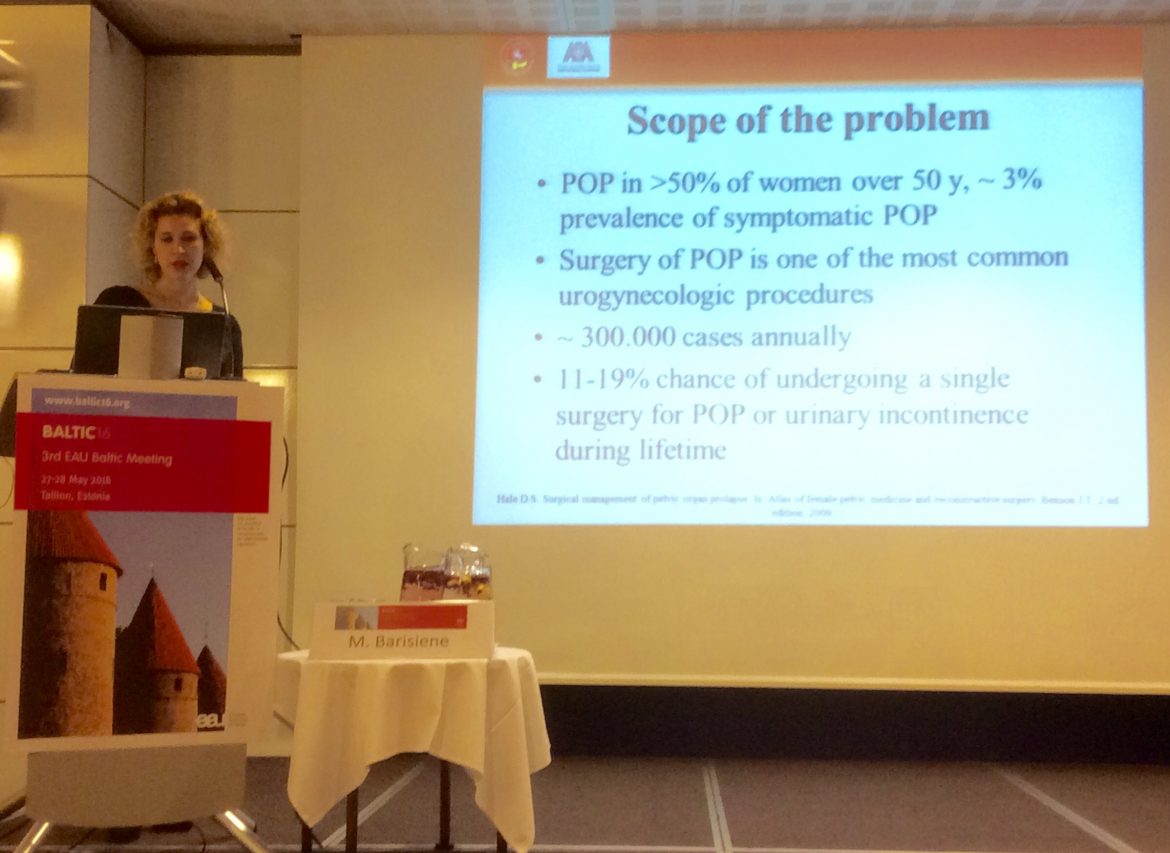
Barisiene discussed pelvic floor reconstruction in women and said the pelvic organ prolapse (POP) occurs in more than 50% of women over 50 years and that POP surgery is one of the most common urogynecologic procedures.
“There is an 11% to 19% chance of undergoing a single surgery for POP or urinary incontinence during a lifetime,” she said adding that in pelvic reconstruction one needs to carefully consider the stage of the problem, overall health and previous surgeries of the patient, surgical expertise and patient’s expectations.
Regarding mesh complications, she the rapid rise in reports of mesh related complications has led to enormous medico-legal problems particularly in the US, and which led the FDA to issue warning statements to doctors and patients. She expects that the new concept for the ideal graft would be degradable materials, permeable to cells and are mechanically robust at the point of implantation.